Jessica Richardson, an associate professor of Speech and Hearing Sciences at The University of New Mexico, has been awarded a five-year, $2 million grant to optimize treatment and interventions for those who acquire the language disorder known as aphasia after suffering a stroke.
Richardson has worked with people with post-stroke aphasia, and other acquired cognitive or communication deficits, for more than 20 years.

“Aphasia is an acquired language disorder that affects speaking, understanding, reading, and writing. All language modalities will likely be affected to some degree, but depending on the type of aphasia, some language modality deficits may be worse than others,” Richardson said. “The most common cause of aphasia is stroke, and about 30-50 percent of people who have had a stroke will live with aphasia for the rest of their lives.”
The grant, awarded from the NIH National Institute on Deafness and Other Communication Disorders, seeks to address the gaps in current treatment options.
“Aphasia is a devastating and debilitating diagnosis. Just imagine not being able to say what you want to say or understand what others are saying, or not being able to read or write anymore. If you think about your everyday life, and what you do every day that involves any type of language, you can begin to understand how big of an impact this can have,” Richardson said. “However, we do know speech-language treatment works and people can continue to recover many years after a stroke.”
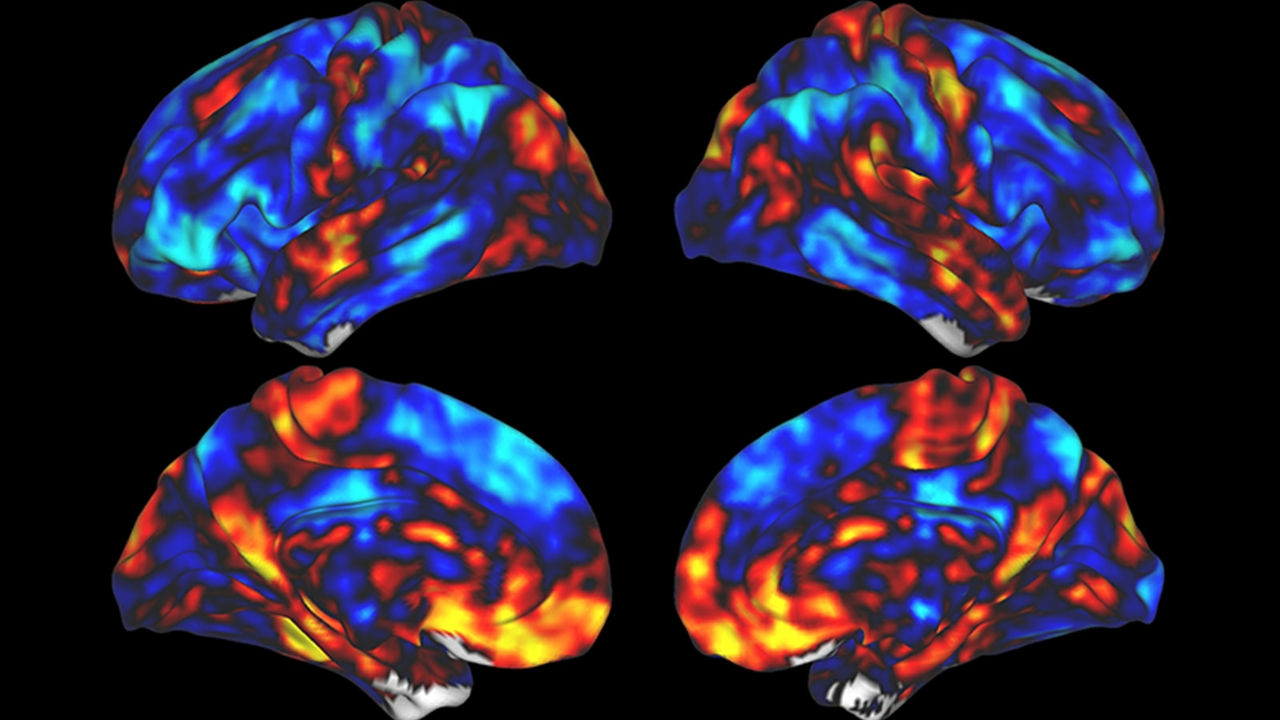
While treatment has been shown to improve aphasia in many patients, Richardson said there is room for improvement. One of the big gaps in current treatment that she seeks to address is not taking full advantage of the brain’s plasticity, or ability to change.
“We know our brain is plastic and very responsive to use or activity. You can change the way the brain works, and even the structure of the brain, with what you do. This is the very foundation of neurorehabilitation. But we have a lot of work to do before it is optimized.”
Richardson said patients with aphasia and their recovery team can help the intact brain repair itself by taking advantage of this plasticity. She hopes to combine evidence-based aphasia treatment with non-invasive brain stimulation for even more optimized treatment.
“We are investigating a non-invasive brain stimulation approach called transcranial direct current stimulation (tDCS). It is thought that you can use this electrical neuromodulation approach, alongside therapeutic activities, to better shape and steer brain changes. Depending on where we place the electrodes on the scalp, we can make neurons more ‘interested’ in a task, as the electrical current may increase the probability that they will send brain signals, or fire,” she said. “We can also tell certain neurons to be quiet if they are interfering in some way, using the electrical current to decrease the probability that they will fire. Over time, with repeated exposure to this, we can potentially change the way the brain functions when ‘doing’ language.”
With this in mind, Richardson and her team are now investigating if the coupling of evidence-based aphasia treatment and brain stimulation can lead to better response to treatment.
This study also is unique, Richardson said, because her team will be aiming to see how this treatment affects narrative language, meaning language in everyday situations, versus a much narrower scope of language, like naming pictured objects, which is often used in most studies of aphasia. The goal is to have a greater impact on the participant’s functional, everyday language abilities.
“We’re looking to see if it improves the ability to produce narratives – descriptions, stories, procedures – which is important because it’s a better representation of how people will communicate in everyday life. If we can show we’re seeing enhancement in narrative and real conversation, it will be a powerful indicator of the effectiveness of this enhanced treatment with tDCS.”
“Each person who has survived a stroke has their own unique brain landscape,” Richardson said. Because of this, she and her team will be using small tDCS electrodes to be more precise about where the electrical current is going, and the dosage of that current, for each individual.
“This is called high-definition tDCS. We will also use EEG to look at the coherence of brain networks to show how well targeted areas are changing their function. This study grew out of pilot work completed at the UNM Center for Brain Recovery and Repair and will involve collaboration with other UNM investigators on both campuses,” she said.
Richardson has worked with people with post-stroke aphasia, or with other acquired cognitive or communication deficits, for over 20 years, and said she has also seen first-hand how particularly devastating aphasia can be, first as a high schooler after her grandfather suffered from aphasia, and more recently with her mother.
“It changes everything about one’s life – identity, autonomy, relationships, financial security… everything. And it changes the lives of the loved ones of survivors as well.”
“We haven’t yet taken full advantage of our brain’s ability to change and we are just now beginning to pay more attention to the parts of the brain often left out of that conversation, the intact areas of the brain versus the damaged. So we are investigating if we could help the undamaged areas work more optimally and be more involved in the behavior we are targeting, for improved outcomes,” Richardson said.
“If we want to change the status quo for rehabilitation for people with aphasia and related disorders, then we need to think very creatively of ways to enhance therapy. This is one of those creative ideas that is based in solid science. Through this grant and other studies in process and in development, we will help to ease at least part of the burden of this disability for some people.”